
VAGINA SHAPES CHANGE BECAUSE OF SKIN
Human papilloma virus (HPV) is the name given to a group of viruses that affect the skin and the moist membranes that line the body, such as those in the cervix, anus, mouth and throat. It's spread during sex, including anal and oral sex. differentiated VIN (dVIN) – this is a rarer type, usually affecting women and anyone with a vulva over 60, associated with skin conditions that affect the vulva.usual or undifferentiated VIN – this usually affects women and anyone with a vulva under 50 and is thought to be caused by an HPV infection.Speak to your GP if you have these symptoms.
Symptoms of VIN are similar to those of vulval cancer, and include persistent itchiness of the vulva and raised discoloured patches. However, because of the risk of cancer, treatment to remove the affected cells is often recommended. In some cases, the abnormal cells may go away by themselves. This is a gradual process that usually takes well over 10 years. This means there are changes to certain cells in the vulva that aren't cancerous, but could potentially turn into cancer at a later date. Vulval intraepithelial neoplasia (VIN) is a pre-cancerous condition. Very occasionally women and anyone with a vulva under 50 can be affected. Most cases develop in women and anyone with a vulva aged 65 or over. The risk of developing vulval cancer increases as you get older. skin conditions that can affect the vulva, such as lichen sclerosus.The exact reason why this happens in cases of vulval cancer is unknown, but certain things can increase your chances of developing the condition. This produces a lump of tissue known as a tumour. This is offered to all girls who are 12 to 13 years old as part of their routine childhood immunisation programme.Ĭancer occurs when the cells in a certain area of your body divide and multiply too rapidly. The HPV vaccination may also reduce your chances of developing vulval cancer. attending cervical screening appointments – cervical screening can detect HPV and pre-cancerous conditions such as VIN.practising safer sex – using a condom during sex can offer some protection against HPV.It's not thought to be possible to prevent vulval cancer completely, but you may be able to reduce your risk by: Radiotherapy and chemotherapy may be used without surgery if you're not well enough to have an operation, or if the cancer has spread and it isn't possible to remove it all. Some people may also have radiotherapy (where radiation is used to destroy cancer cells) or chemotherapy (where medication is used to kill cancer cells), or both. The main treatment for vulval cancer is surgery to remove the cancerous tissue from the vulva and any lymph nodes containing cancerous cells. Read more about the causes of vulval cancer. You may be able to reduce your risk of vulval cancer by stopping smoking and taking steps to reduce the chances of picking up an HPV infection. skin conditions affecting the vulva, such as lichen sclerosus.persistent infection with certain versions of the human papilloma virus (HPV).vulval intraepithelial neoplasia (VIN) – where the cells in the vulva are abnormal and at risk of turning cancerous.The exact cause of vulval cancer is unclear, but your risk of developing the condition is increased by the following factors: Read more about diagnosing vulval cancer. While it's highly unlikely to be the result of cancer, these changes should be investigated. Speak to your GP if you notice any changes in the usual appearance of your vulva. a mole on the vulva that changes shape or colour.

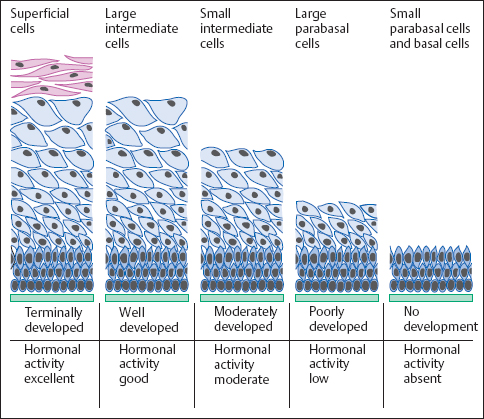
pain, soreness or tenderness in the vulva.The condition is rare in women and anyone with a vulva under 50 who have not yet gone through the menopause. Most of those affected by vulval cancer are older women and anyone with a vulva over the age of 65. It includes the lips surrounding the vagina (labia minora and labia majora), the clitoris (sexual organ that helps reach sexual climax), and the Bartholin's glands (2 small glands each side of the vagina). The vulva is a woman's external genitals. Cancer of the vulva is a rare type of cancer that affects women and anyone with a vulva.


 0 kommentar(er)
0 kommentar(er)
